Adopting An Integrated Treatment Model for Substance Abuse+Trauma
Perspectives and Integrations for human care providers By: Sarah O’Brien, LCSW
Topics covered in this Newsletter:
Adopting an Integrated treatment model for Substance Abuse and Trauma
Integrate’s Trauma-Informed Approach to Community Engagement
Upcoming Community Events
Please get to know our Trauma Informed Professional Community (Subject Matter Experts)
About Sarah O’Brien
Sarah (she/her) is a Licensed Clinical Social Worker (LCSW, LCSW-C),trauma-informed and trained; psychotherapist, substance use/addiction therapist, and she holds specialized certifications in Anxiety treatment and Telemental Health treatment. She is also a writer, creator, advocate, partner of someone with an addiction, and proud dog mama. She founded Rise and Shine Counseling in 2016 after feeling burned out from nearly 9 years serving in public mental health community services boards and hating the system and structure in those places. She started her own practice to do it her way and get away from unrealistic tracking results of clients’ progress. It takes what it takes for folks, and she’s okay with it being a long process at times.
Her clinical experience with adults includes facilitating recovery & relapse prevention groups, providing mental health skill building to an urban mental health population, dually diagnosed individuals, and conducting crisis evaluations and assessments for inpatient hospitalizations. She has also had the privilege of working on an inpatient psychiatric unit in a teaching hospital. Through all these clinical settings, both in urban and rural areas, Sarah has seen trauma affect just about everyone, including herself with early childhood trauma, sexual trauma, and relational/betrayal trauma experiences.
She is passionate about educating others about the effects of trauma on the brain, the body, and social/relational functioning. She has a desire to help others navigate their own stories and struggles to find ways to become their ideal self through psychotherapy, mindfulness, setting boundaries, and finding their safe, supportive network. She also loves to hype and motivate others into increased self-care and ability to affirm themselves and their abilities. She has recently start creating as an outlet to manage stress and overwhelm and it’s turned into making many affirmation stickers for all.Subject Matter Expertise:
Learn more about Sarah’s work as a therapist in Virginia and Maryland
-Neuroscience-based treatment for Anxiety and Panic
-Neuroscience-based treatment for Substance Use/Addiction
-Trauma-Informed Therapy (specifically Relational/Betrayal traumas)
-Social-Emotional Learning and Communication
Introduction
In some ways, healthcare for those with a substance addiction is pretty good. We have treatment centers, inpatient centers, outpatient centers, IOPs, support groups, and medications. Many of the treatment options for managing or releasing substance addiction are covered by health insurance, too. Unlike other compulsive disorders (think eating disorders and obesity/weight management) where insurance refuses to cover medications and often treatment centers, and even outpatient treatment is denied so frequently as an “elective” form of healthcare, rather than the truth:
Addiction and compulsivity show up in many ways, and EVERYONE deserves trauma-informed and appropriate care for their symptoms and health concerns.
Why?
Because these compulsive disorders are often the result of past trauma. And I believe we have a long way to go in the healthcare, and even the mental healthcare, industry to provide ACTUAL care and treatment for these folks. Devaluing or discarding someone because they struggle with some addiction—be it harmful substances like heroin and alcohol, or food (aversions and overeating), or harmful dieting substances and medications—instead of trying to help them, understand them, and care for them. It seems it is way too easy and comfortable for systems, industries, and individuals to devalue and discard… and in doing so, cause further harm, damage, and re-traumatizing the person with the current struggle.
So, I encourage anyone in healthcare—health insurance companies (especially these guys!), hospital systems, outpatient clinics with MDs, PAs, NPs, and psychotherapists—to consider adopting a more integrated treatment model for those individuals with past trauma whose adverse effects ended up being addiction to a substance (vs. cancer vs. Borderline PD vs. crippling anxiety).
Read on to learn what happens in the brain when a person experiences trauma, the adverse outcomes that can be experienced by anyone who has past trauma in their story, why the abstinence/return to use cycle occurs, and what providers can be doing differently to engage more appropriately with this population in need of treatment.
Integrated Treatment Model in Addiction Recovery
What happens in the brain and body when we experience trauma: Under extreme stress, and whether experiencing a single or ongoing traumatic event, both count as extreme stress, “There is a failure of memory processing which results in an inability to integrate incoming input into a coherent autobiographical narrative, leaving the sensory elements of the experience [or trauma] unintegrated and unattached. When activated by current reminders, these sensory elements are then prone to return.” (Van der Kolk, Hopper, & Osterman, 2001).
Research informs that traumatic memories are encoded primarily as bodily and emotional feelings, without words or pictures, leaving a person detached from the event. Sensory elements without words = what’s called implicit memory. Siegel (1999) tells us that “these implicit memories do not carry the internal message that something is being recalled.” Instead, we act, feel, and imagine without recognizing past experiences' influence on our current reality.
The Impact of a Traumatic Experience
Emotional memory takes our past experiences and converts them into an expectation for the future. Also, that dynamic memory makes the worst experiences of our past persist as felt realities in the present. The traumatic event can bring so many things in its wake:
Depression
Irritability
Numbing
Decreased Interest
Decreased Concentration
Insomnia
Shame and Self-Loathing
Physiological Hyperarousal and Psychomotor agitation
Foreshortened Future and/or Hopelessness
Nightmares and/or Flashbacks
Hypervigilance/Easy Startle
Social Anixety
Panic attacks
Chronic Pain and Musculoskeletal issues
Suicidality
Borderline Personality Disorder
Substance Use/Abuse and Compulsivity
The Impact of Trauma Doesn’t Go Away
The traumatic event may be over, but it lives on in implicit memories expressed by folks in the abovementioned ways. Experiencing a traumatic event or events leaves a person responding in such ways, without a desire to, and sometimes without an awareness of, this happening or that they are responding this way because of a traumatic event experienced in the past. Most people can agree on things like insomnia, nightmares, flashbacks, and hypervigilance as “acceptable and understandable” responses to trauma; however, Borderline Personality Disorder, chronic shame and self-loathing, feeling hopelessness about the future AND substance use/abuse (or other issues of compulsivity) are not acceptable and understandable responses to trauma. We often shame and blame folks with addiction for their poor ways of coping and responding to the traumatic events experienced in their life. Maybe there would be less shame and blame if we understood why the cycle of return to use occurs.
For those who struggle with addiction after experiencing trauma, the cycle looks like this:
1. Trauma is activated in survivor’s nervous system by some stimuli
2. Survivor becomes overwhelmed, flooded, impulsive, and desperate
3. Confused, overwhelmed and feeling shame, the survivor blames themselves for what’s
happening in their body (aka the activated nervous system to trauma)
4. This increases feelings of overwhelm, flooding, and unbearable impulses
5. Finally, some compulsive behaviors (like, use of a substance, for example) brings welcomed
relief
6. However, when the “drug effect” wears off, the survivor experiences a rebound effect of activation (to their bodily and emotional feelings in their nervous system) and overwhelm
7. This leads to increasing needs for the survivor to engage in compulsive behavior again, often increasing risk of getting the same desired effect of relief from activation over time (increased substance use or frequency)
8. At this point, the survivor can’t stop the compulsive behavior (aka substance use) because their fear of being overwhelmed by emotion outweighs their fear of consequences from substance abuse. This rebound effect effectually increases the intensity of trauma responses/reactions over time, which leaves the survivor with increased levels of use to manage the higher power of emotional activation/response, and often is the reason folks return to use after periods of abstinence. They become activated in a big way, become flooded and overwhelmed, and return to the compulsive behavior that helped provide relief before.
Make it Make Sense
From a human behavior perspective, this makes total sense! Yet we shame and blame the addict for their behaviors (unrecognized responses to implicit memory activation that only exists inside this person because they have experienced one or many traumas!). Essentially, this person who struggles with addiction AS A RESULT of past trauma likely ONLY works with addiction BECAUSE OF THAT PAST TRAUMA. They likely wouldn’t be struggling with addiction IF they had NOT EXPERIENCED PAST TRAUMA.
So, for decades, our systems have blamed and shamed people with trauma histories. Yes, they have; we have. For lack of understanding about how trauma impacts a person throughout their lifespan and just walking around perpetuating the ‘idea’ that addicts ‘did it to themselves when there is nothing wrong with them, they are addicted to something unhealthy and dangerous now BECAUSE OF WHAT HAPPENED TO THEM in the past. This is backward and we need to do better. Period.
The Trauma-Informed Lens
From a trauma standpoint, the survivor, the person using substances, has created a false window of tolerance, having access only to substances as a means of self-regulation (as in, they were never taught how to recognize their bodily sensations and were never taught how to effectively and in healthy ways regulate their nervous system). They use what they got, what they know, maybe the only thing they ever tried so it’s the only thing they ever know… and it worked, keeps working, so they keep on using it. And after so many repetitions of this cycle and the big rebound effect of more intense symptoms, the person with addiction can’t stop using because the FEAR of OVERWHELMING FEELING is worse than the fear of using a dangerous substance.
Conclusion
Addiction and other self-destructive behavior arise not as a pleasure or punishment—seeking strategy but as a SURVIVAL STRATEGY. (Janina Fisher, 2015). A person using substances to manage nervous system activations from past trauma isn’t doing so to get high, to have a good time, or to punish themselves. They are using the substances because it is/has been the only thing at their disposal to help them manage what’s happening inside their bodies, to survive everyday life, to get anything done, to cope with what’s happened to them.
Reflection
What can providers do differently? To provide support and needed care for these folks.
A few things:
Increase the person’s window of tolerance-work with the body first, before emotions
Increasing the person’s own awareness of their activations- by walking through the events of what occurred, being sure to validate their emotional experiences along the way
Add somatic components to increase mind/body awareness and increase somatic regulation skills
Reframe return to use - ask clients to consider the ‘message’ the return to use was sent to challenge the shame that arises
Increase curiosity and cultivate that in the person, instead of just expressing empathy or confronting the person on their substance use behaviors- the tone of curiosity relaxes defenses and often elicits more information
Being mindful of offering safe, supportive space for the person/client/survivor/person with addiction who has also experienced trauma and also needs to feel seen, heard, and understood—not judged, isolated, and blamed
Moving Toward a Trauma-Informed Lens
Ways to improve our clinical work to support these folks better can:
Validate the relief offered by the addictive behavior
Addressing any of our failure to understand that this person’s fear of relying on people is greater than relying on a substance or behavior that person can control
Addressing your failure to see that one’s life and body are not a priority when your life or body only matters as a vehicle for others to discharge tension, its care becomes meaningless to a person.
Highlighting an understanding of trauma-related shame and secrecy, where “lies” feel “safe and normal” and “disclosure” feels unsafe
We mustn’t get into a power struggle where the therapist/provider is the spokesperson in favor of sobriety, and the survivor/client is the spokesperson in favor of using. Our job is to help the person resolve their internal wars and struggles.
Do you carry unchecked biases about folks struggling with substance addiction? Has it been easy for you to ‘write them off’ due to this response to trauma? What are you willing to do to expand your knowledge about trauma + addiction and how to integrate models of treatment to address both?
Application
Discern two opportunities you can learn to practice making trauma-informed decision-making skills with our Trauma-Informed Decision-Making Table.
Feedback
Tell Sarah if this article impacted you or if you have questions.
Integrate’s Trauma-Informed Community Engagement
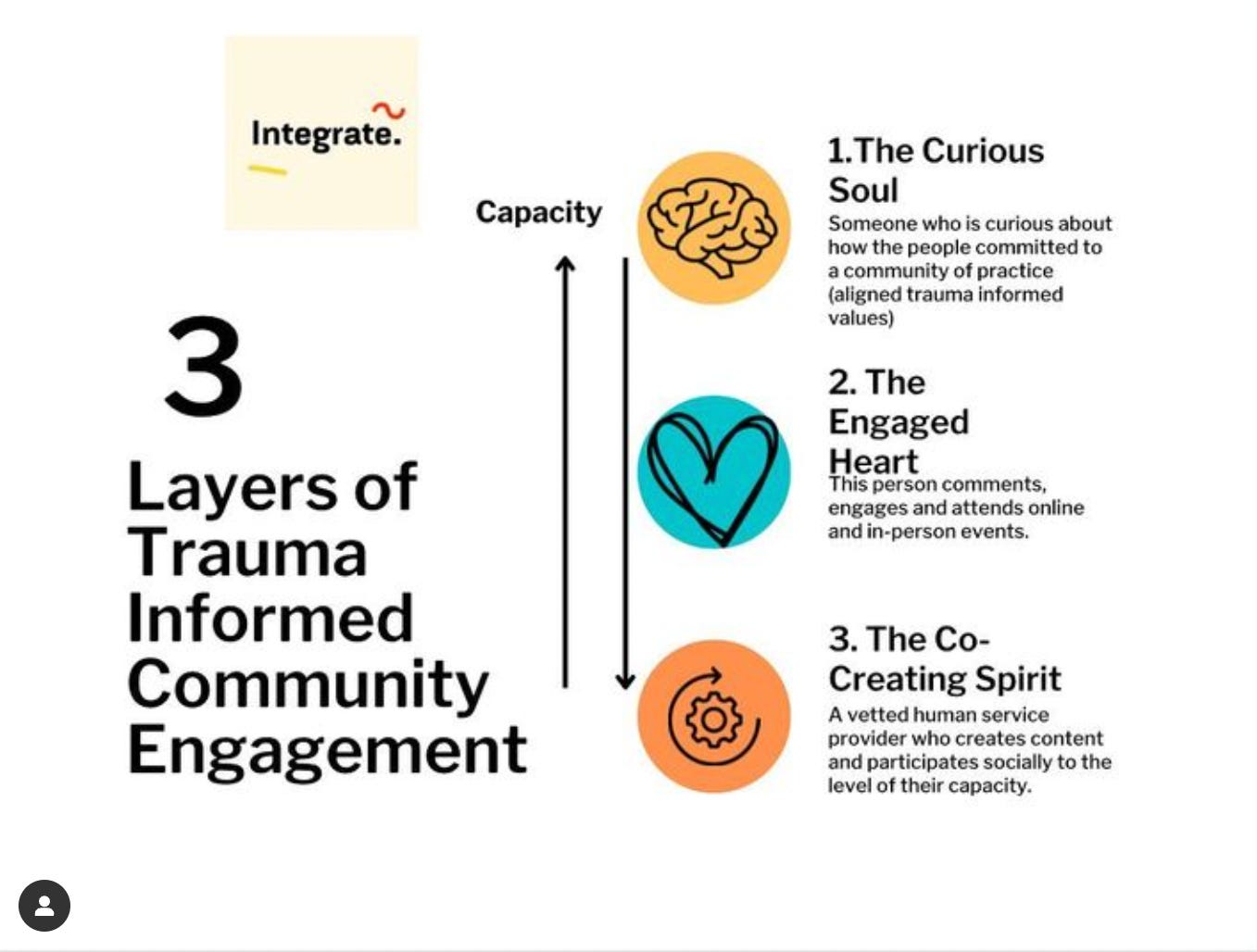
We have been building Integrate as a community of practice around trauma Informed skills for eight years. Over those years, we have observed a beautiful titrated flow we have seen many of our human care providers and survivor community move through as they move through the different chapters of their life.
Like anything else in life, we will move in and out of capacity for engagement. However, regardless of where someone is in the capacity for engagement, we appreciate your presence no matter how distant or engaged you are.
You are valued at every and all levels of engagement.
The three layers to trauma-informed engagement:
Level 1: The Curious Soul
Someone curious about how the people are committed to a community of practice ( aligned trauma-informed values).
Level 2: The Engaged Heart
This person comments, engages, and attends online and in person.
Level 3: The Co-Creating Spirit
A vetted human service provider who creates content and participates socially to the level of their capacity.
Upcoming Community Events
Human-Centered Communication Circle
Trauma-Informed Professionals Q+A
A Panel Discussion on Conscious (Re)parenting
Get to know our community of Trauma Informed Subject Matter Experts (SMES)




